What Is SSRI Withdrawal Syndrome?
The withdrawal syndrome from SSRIs appears when the administration of these drugs is abruptly withdrawn, especially after a treatment of four to six weeks.
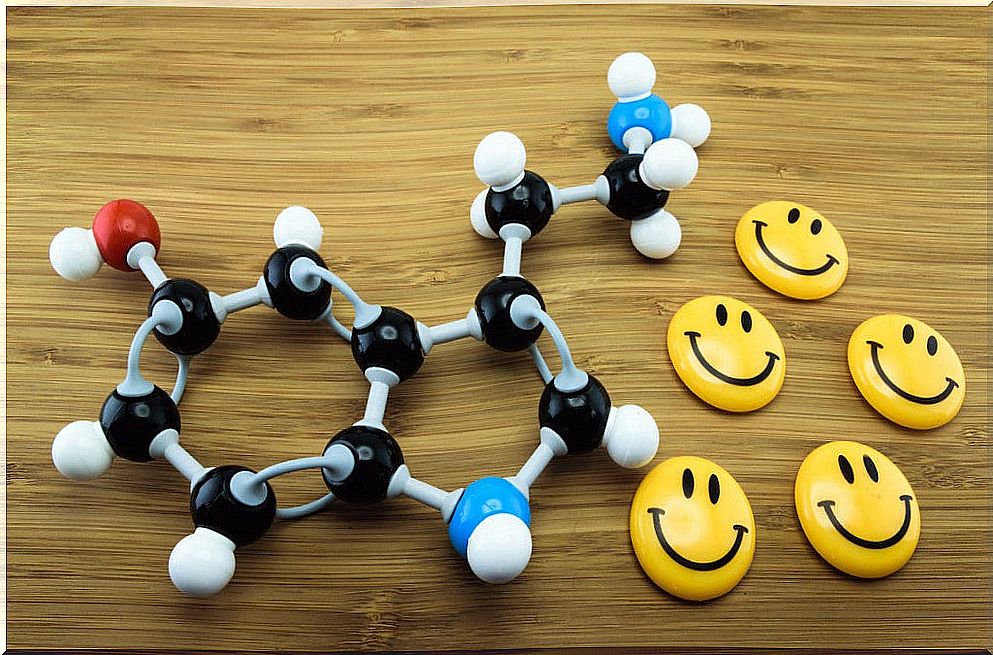
In this sense, the SSRI antidepressant withdrawal syndrome occurs when you stop taking the antidepressant abruptly because the body cannot adapt to this sudden decrease in the level of serotonin in the synaptic space.
SSRIs, selective serotonin reuptake inhibitors, are a group of medications used to treat depression. Serotonin is a substance that nerves use to send messages to each other, a neurotransmitter.
The specific mechanism of action of serotonin reuptake inhibitors is to slow down the reuptake process of this neurotransmitter, by which the nerve cells that secrete serotonin reuptake it.
Symptoms of SSRI withdrawal syndrome
As a result of the sudden increase in serotonin, symptoms of SSRI withdrawal symptoms appear, usually lasting a few weeks. Among the symptoms that may appear are:
- Sickness.
- Tremors.
- Headaches
- Anxiety.
- Sleep disorders and tiredness.
Also, flu-like symptoms such as sore muscles and chills may appear. Another important aspect to keep in mind is that symptoms of depression may reappear after you stop taking an antidepressant. In fact, sometimes it is difficult to differentiate between withdrawal symptoms and depression symptoms.
To minimize your risk of withdrawal from SSRIs, talk to your doctor before you stop taking an antidepressant. Typically, your doctor will recommend that you gradually reduce the dose of the antidepressant over several weeks or more. Thus, your body adapts to the absence of the drug.
However, in some cases, you may be prescribed another antidepressant or other type of medication in the short term to help relieve symptoms. In this way, we help the body adapt little by little to changes.
Evidence on SSRI withdrawal syndrome
An analysis of adverse reactions to SSRIs reported in the UK showed that withdrawal symptoms were reported more frequently with paroxetine than with other group drugs such as sertraline, fluvoxamine and fluoxetine.
Based on these studies, it appears that the variation in the incidence of SSRI withdrawal syndrome is related to the pharmacokinetic characteristics of each antidepressant drug.
Specifically, drugs such as paroxetine, whose elimination half-life is relatively short, over 21 hours, together with the fact that its metabolites are not active, favor the appearance of symptoms of the withdrawal syndrome of SSRIs.
However , with drugs such as fluoxetine it is more difficult for symptoms of SSRI withdrawal syndrome to appear. This is because it has a long elimination half-life, between two and three days. In addition, its metabolites are active and have an elimination half-life of 6 to 9 days.
We must be aware of the possible risk of appearance of the symptoms of this syndrome when antidepressant treatment is stopped abruptly. It is also necessary to consider which antidepressant it is and what pharmacokinetic characteristics it has.
However, when withdrawing any antidepressant from this group, it is advisable to gradually decrease the dose in order to avoid these disorders. Especially with drugs that have a shorter elimination half-life, such as paroxetine.
Conclution
When the administration of a selective serotonin reuptake inhibitor (SSRI) is stopped abruptly, SSRI withdrawal syndrome can occur. The syndrome can manifest itself with symptoms such as vertigo, paraesthesia, tremor, nausea, anxiety, palpitations, sleep disturbances, irritability, agitation, and headache.
Studies indicate that SSRI withdrawal syndrome is more common when antidepressants with a short elimination half-life are abruptly withdrawn, and even more so if their metabolites are inactive.